The intrauterine device, generally known by its initials IUD, is a reversible, temporary and effective contraceptive method widely used by women who want to avoid pregnancy.
Currently, there are two types of IUDs: hormonal and copper. The specialist will be in charge of deciding which is best for each particular patient. In addition, the IUD must be placed by the health care provider and inserted into the fundus of the uterus through the cervix.
Although its mechanism of action is not known exactly, the IUD develops an unfavorable environment inside the uterus for the implantation of the fertilized egg.
The duration of contraceptive protection of the IUD will depend on the type of device in place, and its time of effectiveness usually ranges from 3 to 12 years.
Provided below is an index with the 10 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 2.
- 3.
- 3.1.
- 3.2.
- 4.
- 4.1.
- 4.2.
- 5.
- 5.1.
- 6.
- 7.
- 7.1.
- 7.2.
- 7.3.
- 7.4.
- 7.5.
- 8.
- 9.
- 10.
Types of IUDs
Today, there are two main types of IUDs, one that releases hormones and one that is hormone-free.
- Hormone-free IUD: A plastic structure wrapped in a T-shaped copper wire, although it may also have a circular structure. Some have a center of silver or gold to prevent the breakage of the copper wire.
- Hormonal IUDs work by releasing hormones known as progestins.
Below, we will explain to you the two types of intrauterine devices.
Copper IUD
The copper intrauterine device is made of flexible plastic with a vertical and a horizontal T-shaped branch. The vertical branch is surrounded by a copper wire that prevents sperm from passing through. The effectiveness of this device model begins immediately upon placement.
There are also studies that indicate that the copper of the IUD induces the separation of the head and tail of the sperm, so that they are not able to fertilize the egg.
If you opt for IUD, you should have it checked one month after insertion, then three months after insertion and every year thereafter for as long as the contraceptive effect lasts.
Hormonal IUD
The hormonal IUD, as its name suggests, is a device that releases a small amount of hormones into the body. This type of device prevents pregnancy and helps reduce painful and/or heavy menstrual cycles.
Primarily, there are 3 brands of hormonal IUDs on the market that differ in the duration of their effectiveness:
- Jaydess: 3 years.
- Kyleena: 5 years.
- Mirena: 7 years.
However, it is not necessary for you to have the IUD all these years, as it can be removed at any time.
Mechanism of action
When the uterus detects a foreign body such as the IUD, the release of leukocytes and protaglandins begins. These substances are harmful both to sperm and eggs and to zygotes. Therefore, the introduction of the IUD has both a spermicidal and an abortifacient effect.
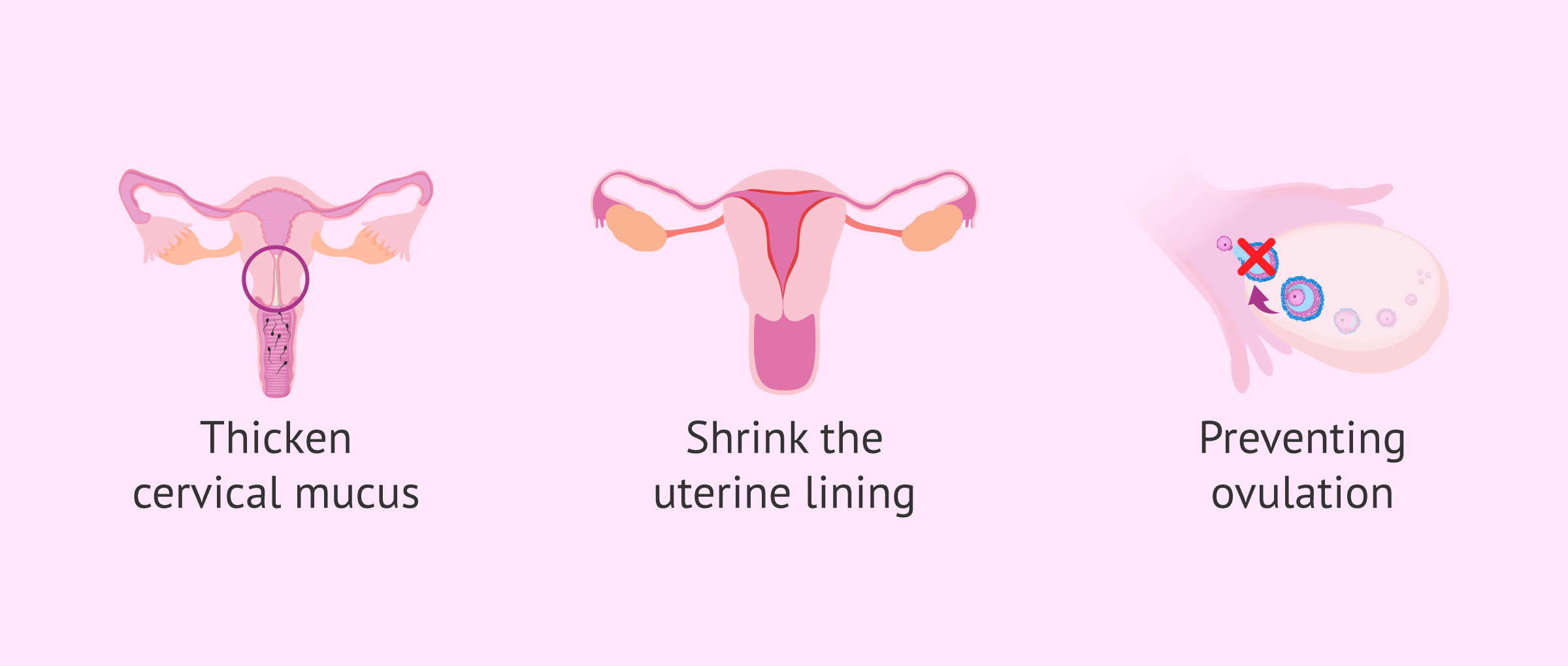
As for the hormonal IUD, the release of hormones continuously over the uterus prevents pregnancy by:
- Thickening the cervical mucus making it difficult to move the sperm.
- Reducing the uterine lining, which decreases the amount and duration of menstrual bleeding.
- Avoiding the release of the egg by the ovary, that is, it prevents ovulation.
The combination of the three mechanisms makes the hormonal IUD highly effective in contraception, although it is generally less effective than other hormonal methods of contraception.
Hormonal IUDs contain only progesterone, unlike other hormonal birth control methods that also contain estrogen. For this reason, the hormonal IUD as well as the copper IUD can be used during lactation.
Keep in mind that neither the hormonal nor the copper IUD prevents the spread of sexually transmitted diseases (STDs).
Use of the intrauterine device
Although the effectiveness of the contraceptive implant is 99%, it is necessary for you to know that it has both advantages and disadvantages.
With this in mind, a balance should be made of the benefits and drawbacks of the IUD when choosing the contraceptive method that best suits each person's personal situation.
What are the advantages of the IUD?
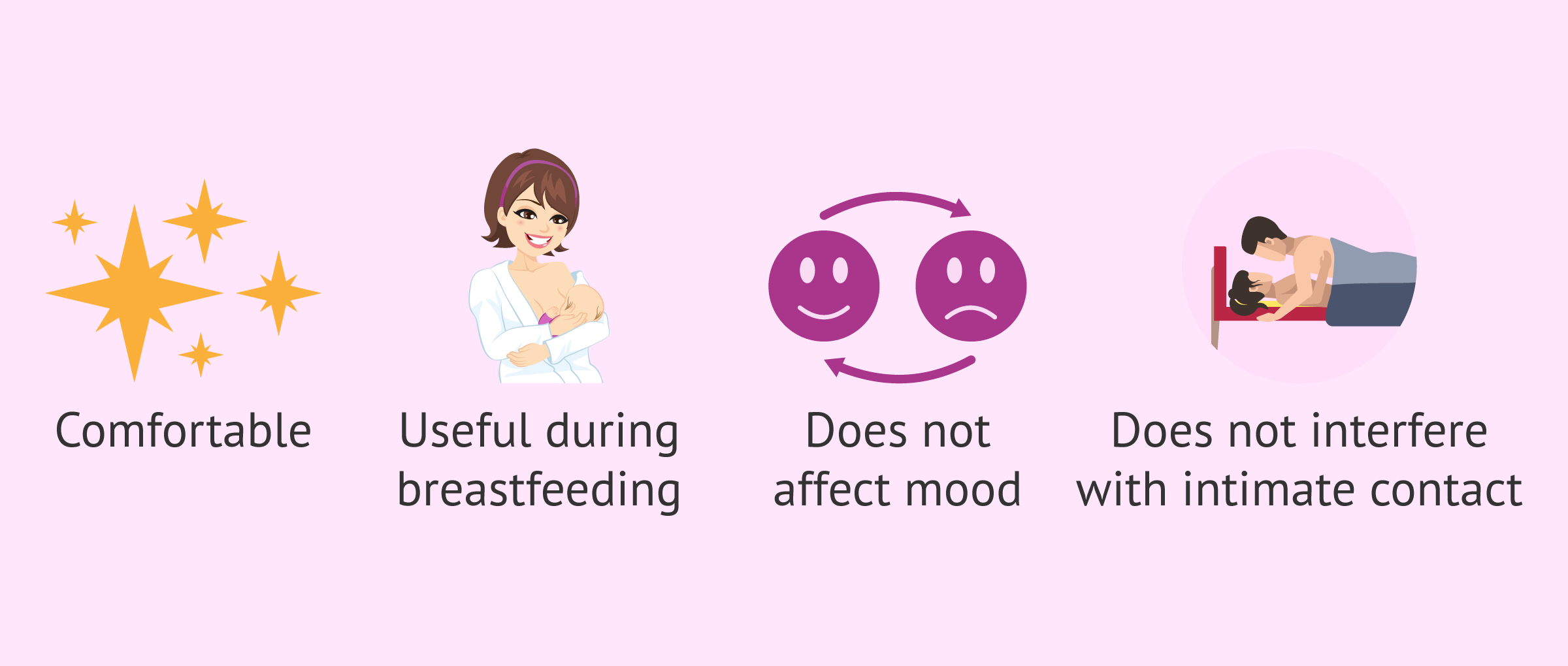
Both the hormonal and copper IUDs offer great comfort, as you can forget about contraception after insertion.
Other advantages of using the IUD include the following:
- It may be used during breastfeeding.
- It can be inserted immediately after an abortion.
- Recovery of fertility just after its withdrawal.
- It usually does not affect mood or sex drive.
- It does not interfere with intimate contact.
It should be noted that, depending on the type of IUD, there may be other advantages for each individual woman.
Disadvantages
Although there are many advantages, the contraceptive implant is not always the ideal method for everyone because it has disadvantages. Here are some of them:
- Pain during insertion
- It does not prevent the spread of STDs and may even increase the risk of STDs because it promotes inflammation.
- It can't be employed by all women.
- It requires a specialist for placement and removal.
- Risk of ectopic pregnancy.
- It can be spontaneously expelled by the body.
- May cause back cramps and pain.
Ultimately, the specialist should provide you all the information necessary before inserting the IUD.
Placement and removal of the DIU
The insertion and removal of the contraceptive implant is very important to be performed by a gynecologist.
Placement
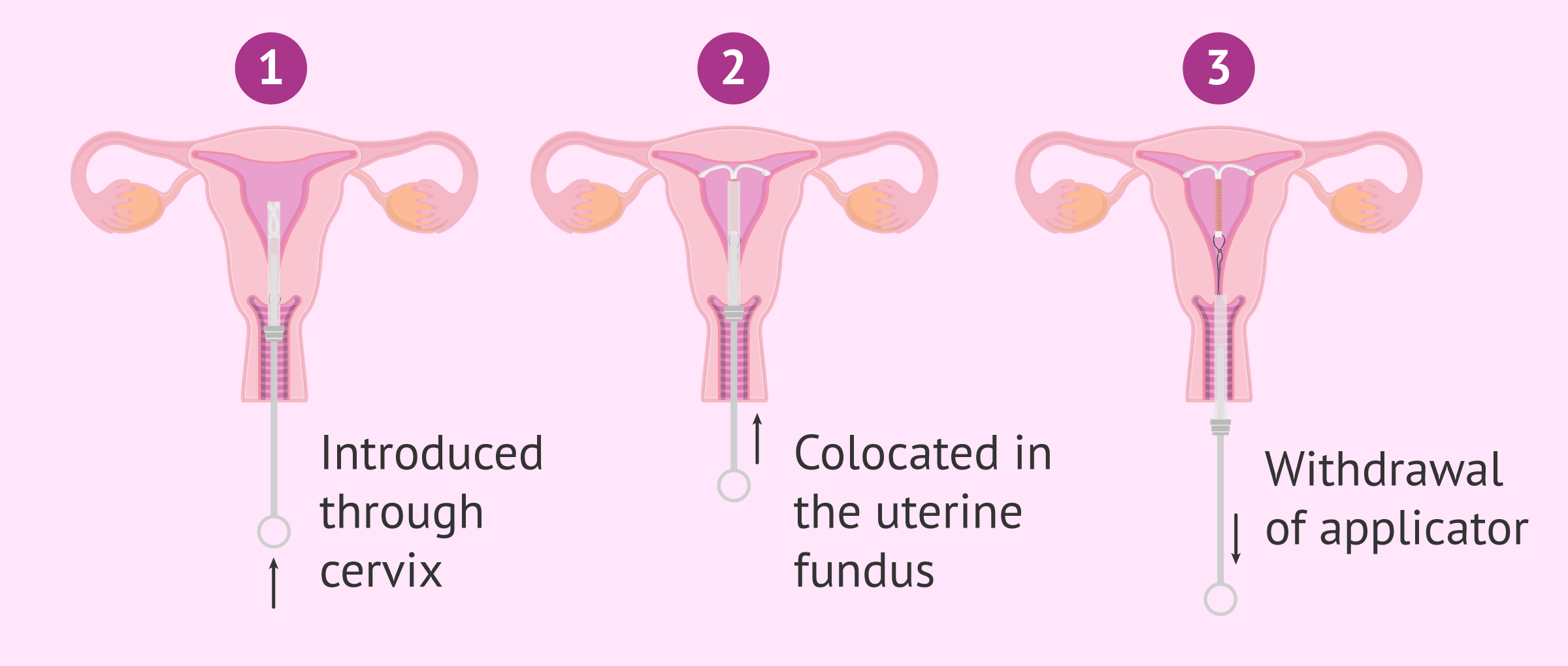
Once the gynecologist has ensured that the IUD is the most appropriate contraceptive method for you based on you gynecological history, it will be inserted at the clinic. This process is simple, can last between 15 and 20 minutes and does not require anesthesia.
For this purpose, you'll be lying down in a gynecological position with your legs slightly open and the doctor inserts the IUD into the uterus through the vagina with the help of an applicator. Once inserted, the specialist leaves a string inside the vagina to indicate that the IUD is correctly inserted and removes the applicator.
Of course, you can change your mind at any time and the medical professional will simply remove the IUD.
Withdrawal
The IUD removal process is quick and simple. The qualified specialist places the speculum to widen the vagina and have a better view of the cervix. He will then insert ring forceps so that he can pull the cord carefully, the arms of the IUD are folded, and removed. You may feel some pain as the IUD comes out.
If your doctor tries to remove the IUD without success, he can use a cyto brush. This is a small brush that is inserted, rotated, and then removed again by grasping the retracted or difficult strings of the IUD and removing the device. In addition, in more complicated cases, removal of the IUD may require outpatient surgery.
In case you have unprotected sex in the weeks before IUD removal, you might become pregnant. This is because sperm live up to 5 days inside a woman's body.
After the IUD is removed, its contraceptive effect quickly disappears and you might become pregnant.
What are the side effects of the IUD?
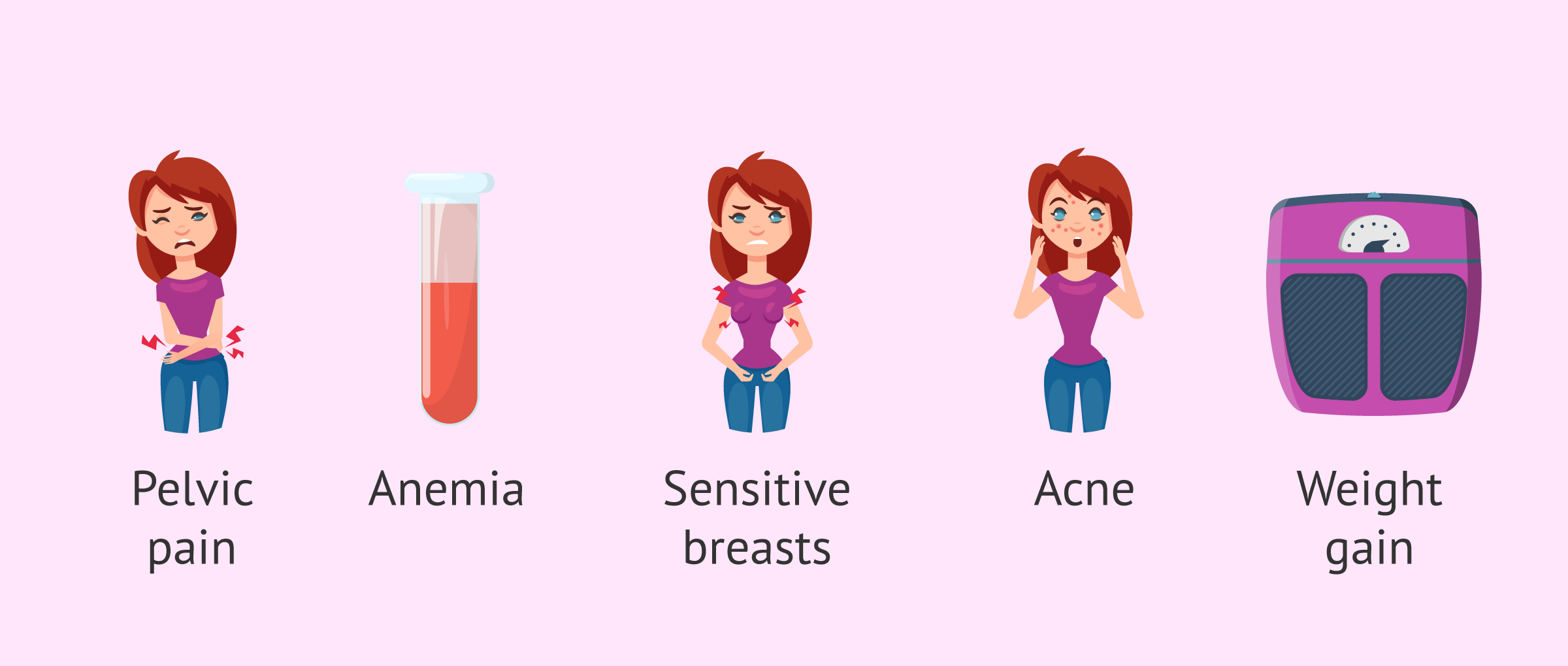
The most common side effects of the IUD are bleeding changes, such as irregular, prolonged, and/or heavy bleeding during the first few months. Other secondary symptoms that may appear in women in the short term due to the use of the implant are the following:
- Pelvic pain
- Anemia due to blood loss.
- Headache and migraine.
- Sensitive breasts.
- Acne.
- Weight gain.
- Itching, redness, or swelling of the vagina.
Typically, these symptoms usually disappear within 3 to 6 months after IUD insertion, once the body becomes used to having the device in the uterus.
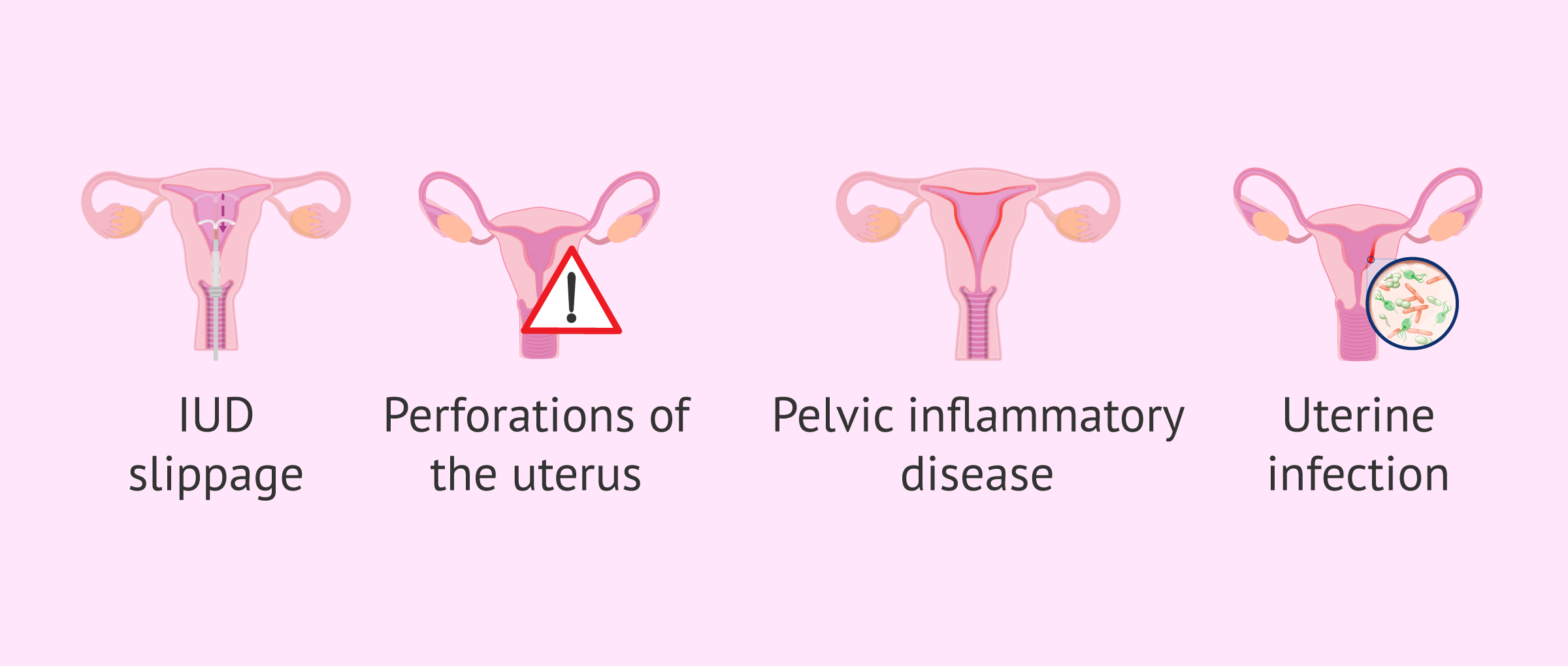
Complications of IUD use
Serious IUD problems are rare, but not impossible. Therefore, some complications that may arise are:
- Expulsion or slipping of the IUD out of the uterus.
- Perforation of the uterus during insertion.
- Pelvic inflammatory disease
- No visualization of the wires.
- Infection of the uterus.
In short, the IUD is a safe and effective method of birth control, but regular medical follow-up is essential. We also recommend you to see a specialist should you notice any alarming symptoms.
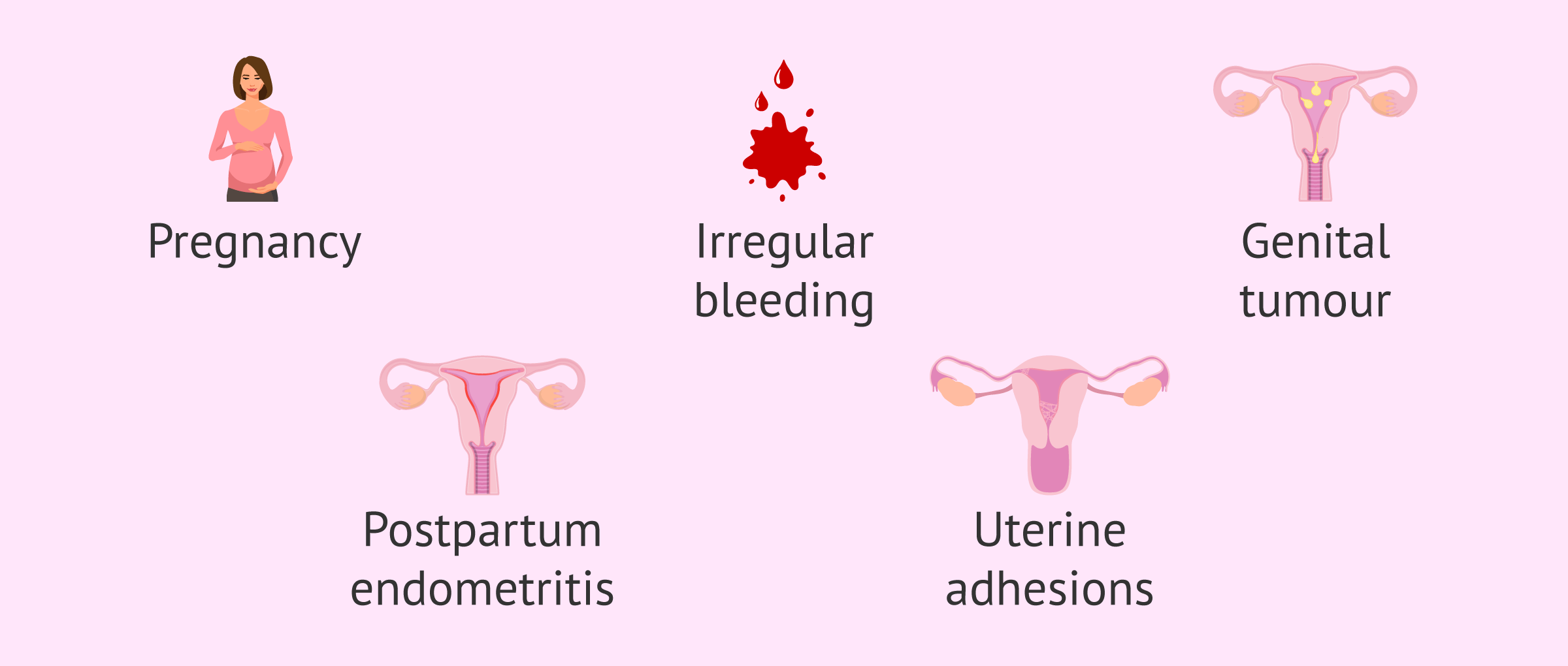
Contraindications of the DIU
The contraindications of the intrauterine device are scarce but should not be forgotten. Some of them are discussed below:
- Pregnancy. However, sometimes the IUD is used as emergency contraception in the first 48 hours. This means that the IUD can be inserted up to 48 hours after unprotected sex and to protect against pregnancy.
- Irregular bleeding with no known cause.
- Suspicion of genital tumor.
- Postpartum endometritis or endometriosis.
- Presence of uterine adhesions.
IUDs should also not be considered for women who have recently had a pelvic infection or whose uterus has abnormal measurements, either because it is too large or too small.
FAQs from users
Can the IUD lead to fertility problems in the future?
The intrauterine device (IUD) is a contraceptive method that after removal should not lead to fertility problems. Most studies and clinical practice show this.
There is little chance that the IUD is a risk factor for a low genital infection (infections that develop in the vagina and/or cervix) to ascend into the uterine cavity, the fallopian tubes, and eventually the abdominal cavity. This is why it is so important to carry out periodic check-ups of the IUD and to see a gynecologist if any type of symptom appears that could be related to it.
Can IUD be inserted while on menstruation?
The IUD can be inserted at any time during a woman's menstrual cycle. If it is inserted when a woman has her period, it is good because she would be unlikely to be pregnant. It is also easier to insert. During menstruation, however, it is not so easy to see signs of infection.
At what age can the IUD be used as birth control?
The IUD can be offered to any woman, including adolescents who have problems with other contraceptive methods. There is no age limit, as long as the woman is not at risk.
What happens if the IUD is expiring?
Once the end date of the IUD is reached, its contraceptive effectiveness decreases over time.
What is the price of the IUD?
The price of a copper IUD is between 35 and 50 euros, while a hormonal IUD costs between 100 and 200 euros approximately.
However, in many Autonomous Communities of Spain the IUD is subsidized.
Suggested for you
In addition to the IUD, there are other contraceptive methods. If you want more information about them, I recommend you read the following article: Contraceptive methods: types, effectiveness, risks and prices.
Apart from that, we have commented that one of the contraindications for inserting the IUD is endometriosis. If you want to know more about endometriosis, click here: What is endometriosis?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Adeyemi-Fowode OA, Bercaw-Pratt JL. Intrauterine Devices: Effective Contraception with Noncontraceptive Benefits for Adolescents. J Pediatr Adolesc Gynecol. 2019 Sep;32(5S):S2-S6. doi: 10.1016/j.jpag.2019.07.001 (View)
Apter D. International Perspectives: IUDs and Adolescents. J Pediatr Adolesc Gynecol. 2019 Sep;32(5S):S36-S42. doi: 10.1016/j.jpag.2019.04.009 (View)
Bastin A, Scanff A, Fraize S, Hild JC, Lous ML, Lavoue V, Ruelle Y, Chaaban S. Direct vs. standard method of insertion of an intrauterine contraceptive device: insertion pain and outcomes at 6 months. Eur J Contracept Reprod Health Care. 2019 Oct;24(5):399-406. doi: 10.1080/13625187.2019.1659951 (View)
Espey E, Yoder K, Hofler L. Barriers and Solutions to Improve Adolescent Intrauterine Device Access. J Pediatr Adolesc Gynecol. 2019 Sep;32(5S):S7-S13. doi: 10.1016/j (View)
Hunter TA, Sonalkar S, Schreiber CA, Perriera LK, Sammel MD, Akers AY. Anticipated Pain During Intrauterine Device Insertion. J Pediatr Adolesc Gynecol. 2019 Sep 26. pii: S1083-3188(19)30306-7. doi: 10.1016/j.jpag.2019.09.007 (View)
Lei Y, Iablakov V, Karmali RJ, Forbes N. Endoscopic Removal of Migrated Intrauterine Device: Case Report and Review of Literature and Technique. ACG Case Rep J. 2019 Jun 20;6(6):e00090. doi: 10.14309/crj.0000000000000090 (View)
Soto F, Delgado AE, Becerra ML, Guillamón M, Jiménez S. DIU en atención primaria. Elsevier. 2003 Vol 41 (3). 162-169 (View)
Ulbricht S, Beyer A, John U. Association between the use of free-of-charge intrauterine devices and a history of induced abortion: a retrospective study. BMC Womens Health. 2019 Oct 18;19(1):120. doi: 10.1186/s12905-019-0821-3 (View)
Zaconeta AM, Oliveira AC, Estrela FS, Vasconcelos TM, França PS, Wanderley MDS, Amato AA. Intrauterine Device Insertion during Cesarean Section in Women without Prenatal Contraception Counseling: Lessons from a Country with High Cesarean Rates. Rev Bras Ginecol Obstet. 2019 Aug;41(8):485-492. doi: 10.1055/s-0039-1693677 (View)
FAQs from users: 'Can the IUD lead to fertility problems in the future?', 'Can IUD be inserted while on menstruation?', 'At what age can the IUD be used as birth control?', 'What happens if the IUD is expiring?' and 'What is the price of the IUD?'.