INTRODUCTION
Total hip arthroplasty (THA) is considered one of the most successful procedures developed during the last century, with excellent long-term results. Worldwide, increasingly younger and more active patients with osteoarthritis are being treated, demanding increasing levels of postoperative clinical function and the ability to engage in physical activity[1]. In Europe, over 20% of all patients treated with THA are under the age of 60 years[2]. The demand for surgical procedures and implants that allow for an active, high-quality, daily life continues to grow. Minimally invasive techniques are on the rise, allowing for the performance of muscle- and soft-tissue-sparing implantations. In contemporary THA, in addition to choosing the right approach, the choice of implant can potentially determine the postoperative outcome. Selecting an adequate femoral implant strongly contributes to the optimal use of minimally invasive techniques[3].
To date, four types of femoral implants are available for THA: hip resurfacing, conventional straight stems, anatomical shortened conventional stems, and short stems.
Hip resurfacing has been introduced as a bone-sparing alternative to conventional THA, associated with a reduced risk of dislocation, easy replication of hip biomechanics, and easier revision, if necessary[4]. However, problems with femoral head necrosis and osteolysis caused by wear and metallosis caused by metal-on-metal bearing couples have resulted in a strong decline in the implantation numbers. The unrestricted use of this technique cannot currently be recommended[5].
Although excellent long-term survival rates have been reported with the use of conventional femoral stems in THA, proximal stress shielding and thigh pain often occur after THA[6-8]. In younger patients, who will likely require eventual revision surgery, the conservation of proximal bone mass and extended service life are preferable for femoral implants. Additionally, minimally invasive techniques may be adversely affected using conventional stems[3].
Short stems have become increasingly popular in recent years. Short-stem THA aims to preserve bone, prevent stress shielding, and provide favorable conditions for revision without altering the basic concepts of conventional THA. Most short-stem designs focus on metaphyseal fixation. Short femoral stems were previously developed decades ago to ensure a bone- and soft-tissue-sparing implantation approach; however, in recent years, numerous innovations and modifications have emerged on the market[9]. However, some short-stem designs have already been withdrawn from the market for a variety of reasons. In Europe, the concept of short-stem THA has become increasingly important, and implantation numbers increase yearly. For example, in Germany, 10.4% of all primary THA procedures are performed using a cementless short stem[10]. However, a large variety of short stem models are available, which differ in both design and function[11].
For most new-generation short-stem designs, short- and mid-term results have been reported[12-15]. At present, however, little data is available regarding long-term outcomes[16]. A major concern in reducing length and diaphyseal fixation of the femoral component is the concomitant reduction of implant stability and the increase of interface micromotion. By interfering with osteointegration, the long-term risk of implant loosening might increase as well[17,18]. Also, positive effects on bone remodeling and stress shielding in the long term have yet to be demonstrated for many short-stem designs[19].
The concept of modern calcar-guided short stems in THA aims for the precise reconstruction of the individual, anatomic hip geometry, using a bone- and soft-tissue sparing implantation technique associated with a physiological loading in the meta-diaphysis to conserve proximal bone stock over the long term. This new-generation short stem design allows for the reconstruction of the individual patient’s anatomy by following the calcar of the femoral neck[20]. Meta-diaphyseal anchoring is applied, consisting of either pronounced metaphyseal anchorage alone or with additional diaphyseal anchorage, depending on the stem alignment and indication[15,21]. The classification of this stem design therefore is challenging; however, in Europe, the term “calcar-guided” has become established in recent years[22] (Figure 1).
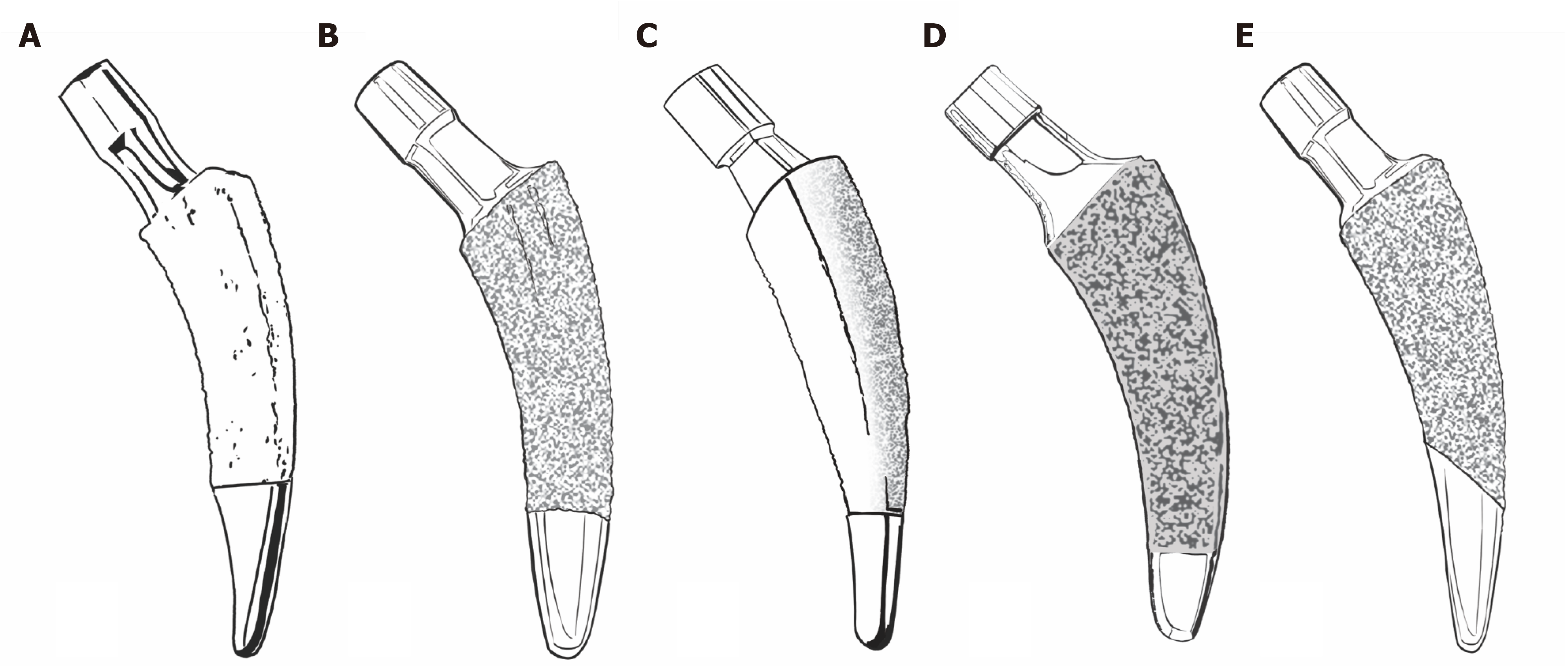
Figure 1 Common new-generation calcar-guided short stems.
A: Nanos stem (Smith&Nephew, Marl, Germany; on the market since 2004); B: MiniHip stem (Corin, Cirencester, UK; on the market since 2007); C: ColloMIS stem (Lima Corporate, Villanova di San Daniele del Friuli, Italy; on the market since 2009); D: optimys stem (Mathys Ltd., Bettlach, Switzerland; on the market since 2013); E: A2 stem (Artiqo, Luedinghausen, Germany; on the market since 2016).
CLASSIFICATION
An early classification system for short stems in THA was proposed by Jerosch[23] and adjusted by Falez et al[11]. This system is based on the corresponding level of the femoral neck resection, differentiating between neck-retaining, partially neck-retaining, and neck-resecting short stems. Distinctions in terms of biomechanics and implantation techniques are also considered. Another recent classification system, described by Khanuja et al[24], was introduced in 2014. This system categorizes all short-stem designs into four groups, in addition to subgroups. The group of partially neck-retaining stems defined by Jerosch comprises the group of calcar-loading stems defined by Khanuja et al[24] (Group 2). A subclassification method was added, dividing calcar-loading stems into trapezoidal, rounded, threaded, and thrust-plate designs. Modern calcar-guided short stems are almost exclusively classified as trapezoidal, rounded, calcar-loading stems according to the system defined by Khanuja et al[24] (Groups 2A and B). The newest generation of contemporary short stems consists almost exclusively of calcar-guided and calcar-loading short stems, such as the Nanos stem (Smith&Nephew, Marl, Germany), the MiniHip stem (Corin, Cirencester, UK), the ColloMIS stem (Lima Corporate, Villanova di San Daniele del Friuli, Italy), the optimys stem (Mathys Ltd., Bettlach, Switzerland), and the A2 stem (Artiqo, Luedinghausen, Germany) (Figure 1). All of these stem designs can be anchored either by metaphyseal anchorage alone or with the addition of diaphyseal anchorage, depending on an individualized positioning. Thus, classification depends not only on the design features but also on the positioning.
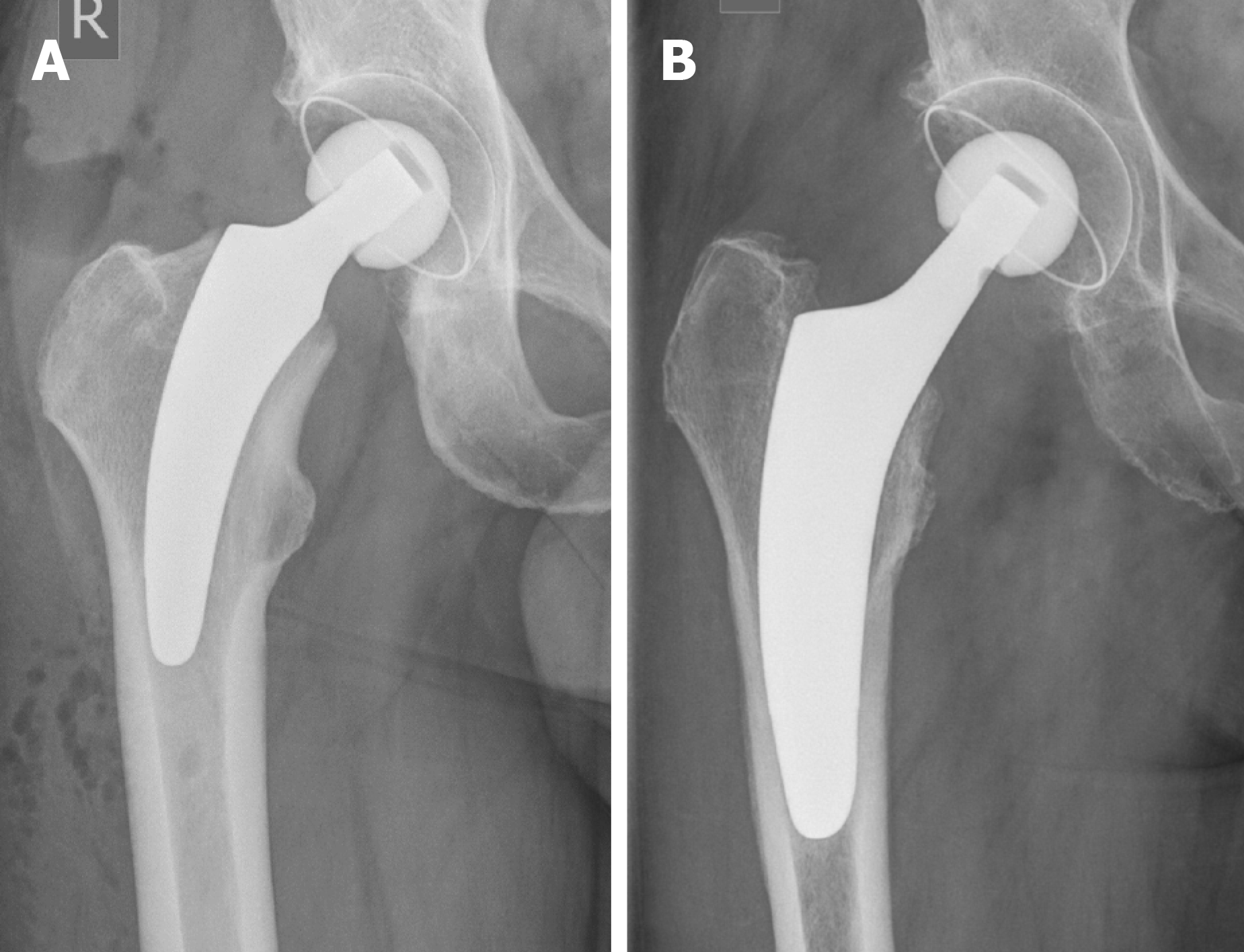
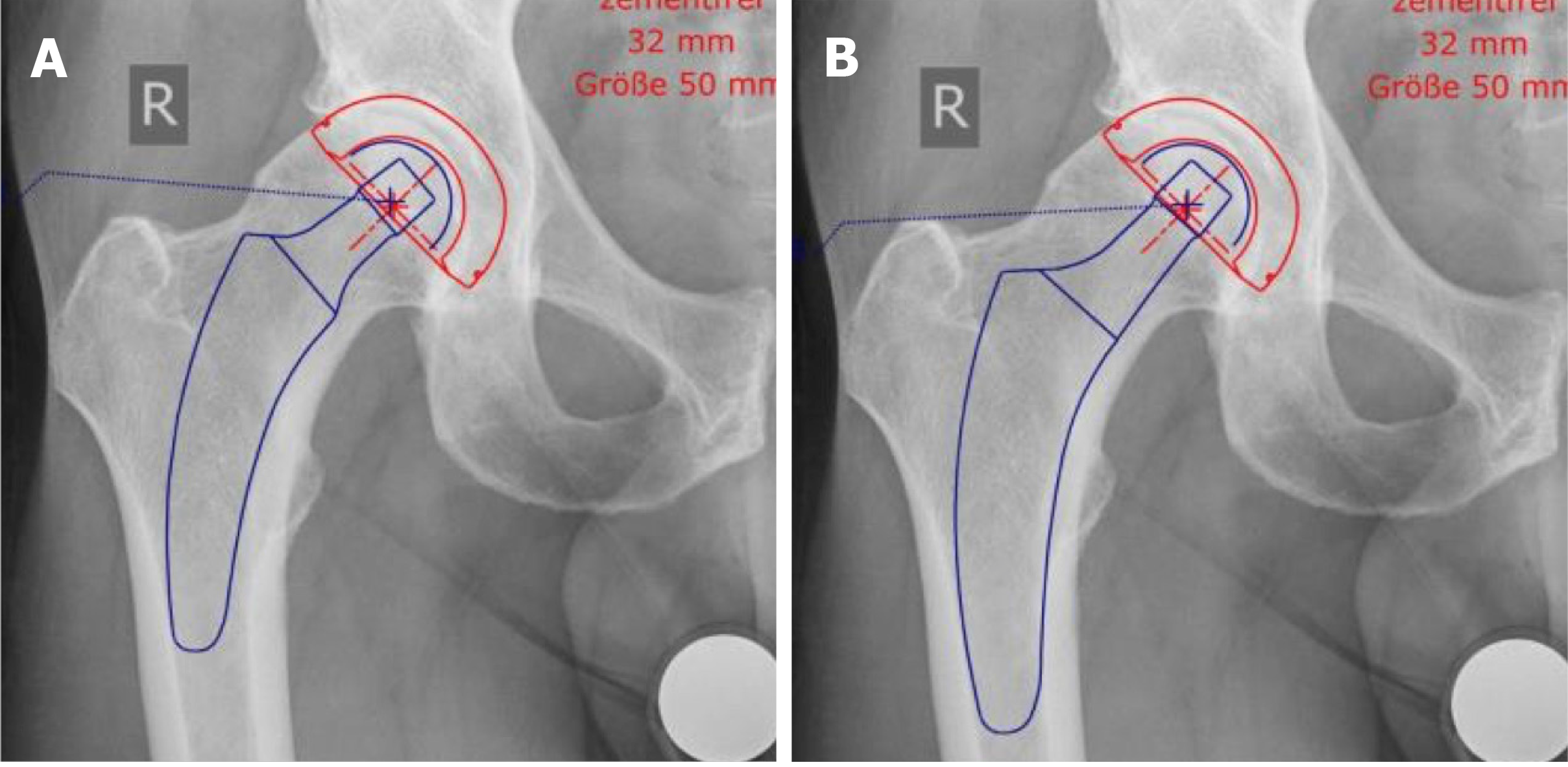
To account for differences in the individualized positioning and anchorage of calcar-guided short stems, a second subclassification method is suggested, distinguishing metaphyseal anchorage [for example Group 2B(M)] from meta-diaphyseal anchorage [Group 2B(MD)], for all stems summarized in Group 2B (Figure 2A and B).
Figure 2 Introduction of a subclassification to account for the individualized positioning of group 2A and 2B stems, according to Khanuja etal[24].
A: Metaphyseal anchorage [for example group 2B(M)]; classical three-point anchoring; B: Meta-diaphyseal anchorage [group 2B(MD)]; additional fit-and-fill in the proximal diaphysis. Citation: Khanuja HS, Banerjee S, Jain D, Pivec R, Mont MA. Short bone-conserving stems in cementless hip arthroplasty. J Bone Joint Surg Am 2014; 96: 1742-1752.
RECONSTRUCTION OF THE ANATOMY
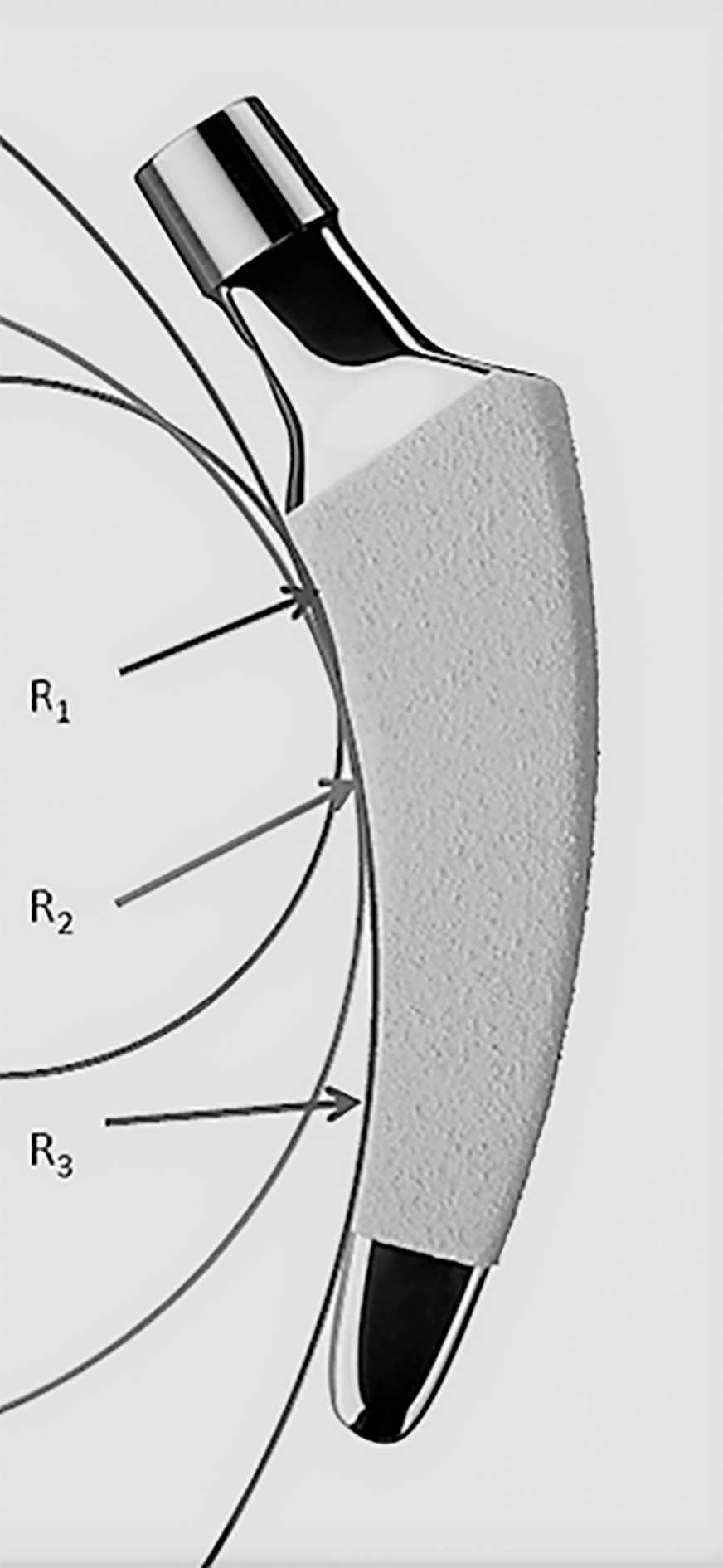
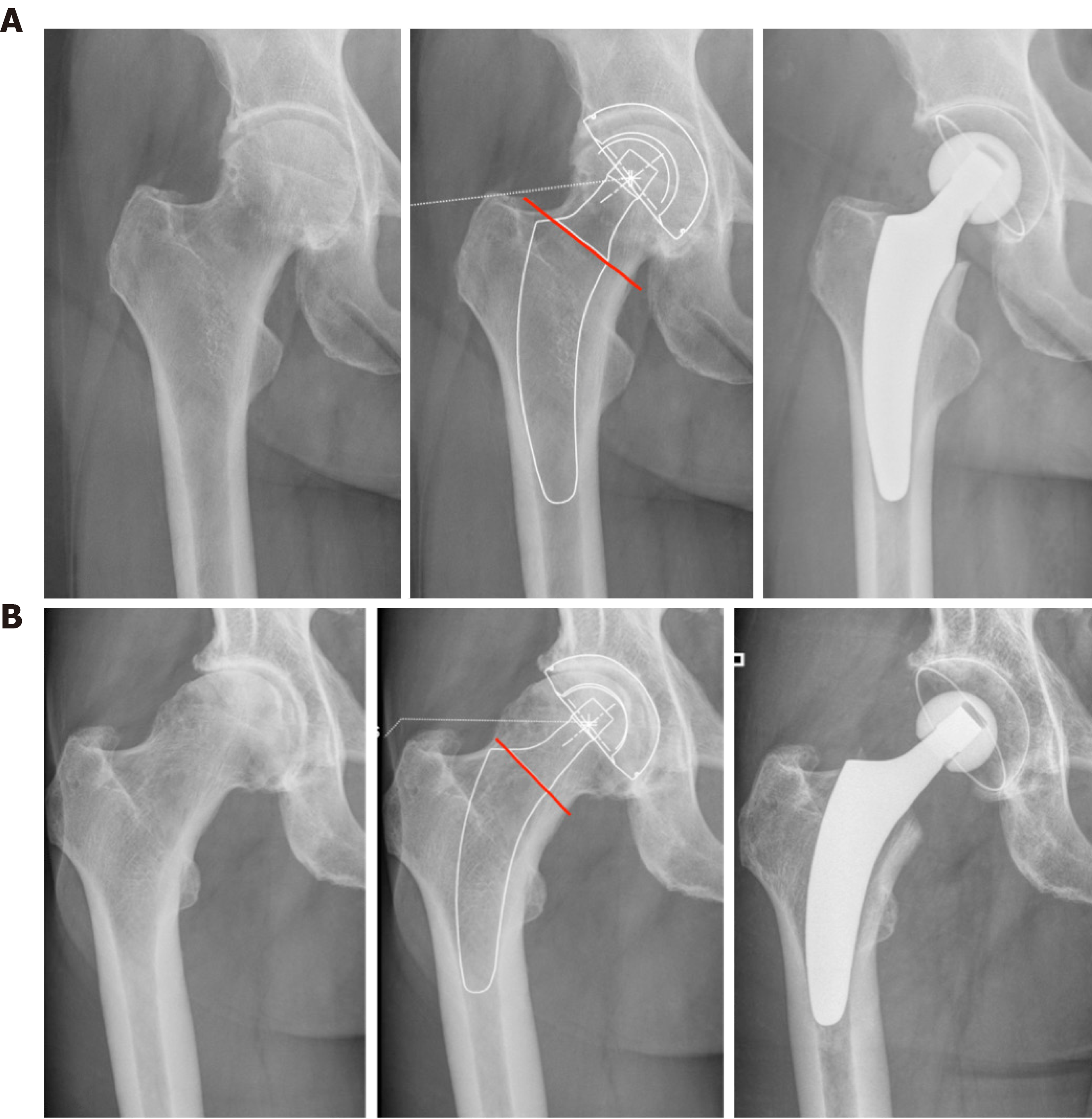
The design of modern calcar-guided short stems features a characteristically rounded shape that can be adapted to the medial anatomical calcar curve (Figure 3). The positioning is performed according to the individual anatomy along the calcar curve[20]. It is dependent on the resection level of the femoral neck. This feature differentiates this design from other conventional stems and many other short-stem designs. Calcar-guided short stems can follow a valgus anatomy into a valgus position or a varus anatomy into a varus position. The positioning must be accomplished by the surgeon, through the intraoperative selection of an individualized, adjusted level of resection, according to the preoperative plan (Figure 4A and B). A high resection of the femoral neck leads to a varus position, with a corresponding high offset, whereas a low resection results in a valgus alignment and a corresponding low offset[20]. It has been demonstrated that the individual anatomy of the proximal femur can, therefore, be reconstructed across a broad bandwidth and offset, allowing leg length to be restored[25-27]. Kutzner et al[21] introduced a classification divided into Groups A–E, in which Groups A and B represented varus anatomies, Groups C represented a neutral hip, and Groups D and E represented valgus anatomies, based on the caput collum diaphysis (CCD) angle. A stem design with an anatomical calcar fit has been reported to be advantageous for preventing unwanted valgization[28]. Additionally, in the second plane, the natural anterior tilt of the femoral neck can only be preserved by a short femoral implant, without needing the application of high antetorsion, facilitating the restoration of both lateral and anterior offset[29] (Figure 5).
Figure 3 The design of modern calcar-guided short stems, with a rounded shape, is adapted to the medial anatomical calcar curve.
In the case of the optimys stem (Mathys Ltd., Bettlach, Switzerland), three different radii were used to design the curve (R1-3). (Copyright Mathys Ltd., Bettlach, Switzerland).
Figure 4 Individualized levels of resection, according to preoperative planning.
A: Valgus anatomy; B: Varus anatomy.
Figure 5 The natural anterior tilt of the femoral neck (in the second plane) can only be reconstructed using a short stem.
SPARING THE BONE AND SOFT TISSUE
Due to the short and rounded design, the insertion of the instruments and the implantation itself is performed using a ‘round-the-corner’ technique, which spares the greater trochanter region[30]. This conveniently avoids the potential fracturing of the trochanter and also reduces the damage to muscle and soft tissues that insert at the piriformis fossa and the greater trochanter, such as the crucial gluteal muscles. Compared with the implantation of conventional implant designs, more proximal femur bone mass can be preserved during short stem implantation surgery[31]. Minimally invasive approaches, without transection or damage to the muscles, are clearly facilitated by the use of this technique (Figure 6). Recent studies have indicated that calcar-guided short stems are advantageous compared with conventional stem designs in terms of intraoperative blood loss and the rates of blood transfusion[32]. In general, the design features of calcar-guided short stems are particularly suitable for minimally invasive approaches[30].
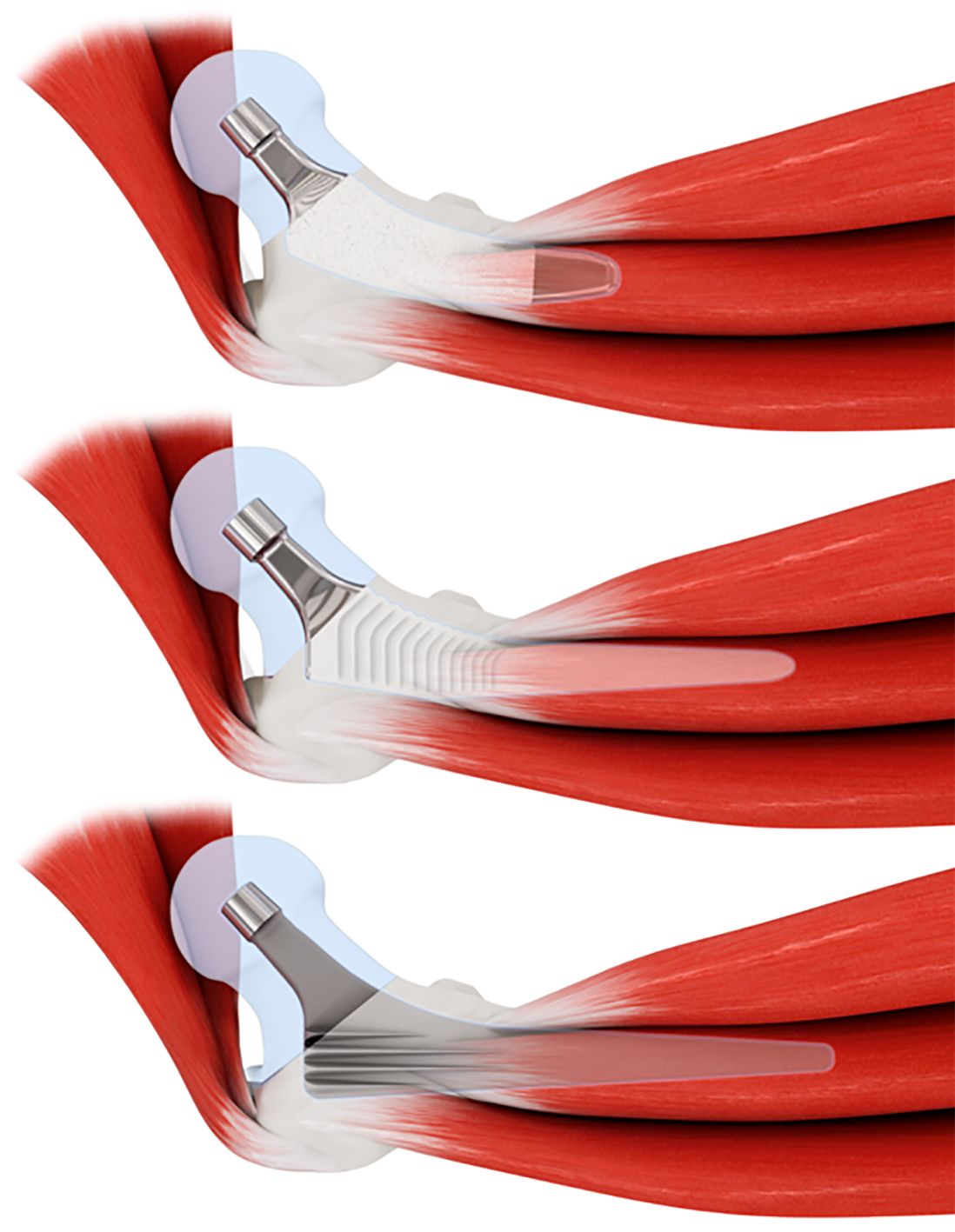
Figure 6 Using rounded short stems (top), minimally invasive approaches, without requiring transection or damage to the muscles, are facilitated compared with conventional stems (middle and bottom).
Copyright Mathys Ltd., Bettlach, Switzerland.
ANCHORAGE
The primary concept of short stems focuses on anchoring in the metaphysis. Most short-stem designs use three-point anchoring to achieve a stable primary fixation (Figure 7A–C). The first short-stem design to pursue this philosophy was the Mayo stem (Zimmer Biomet, Warsaw, Indiana, USA), which was introduced in 1985 and is no longer available on the market (Figure 7A). The pronounced metaphyseal anchorage aimed to achieve the physiological loading of the proximal femoral bone. The minimization of stress shielding is preferable[21,33]. The preservation of bone stock is considered to be beneficial in case future revision surgery is necessary[31]. A popular and widespread representative of the metaphyseal anchoring philosophy is the Metha stem (Aesculap, Tuttlingen, Germany) (Figure 7B). The design features of this stem in the distal part do not easily accommodate an additional diaphyseal anchorage, which is almost impossible to attain during surgery, even in neutral or valgus anatomies (Figure 8A). Therefore, a strictly non-compromised proximal bone stock and sufficient bone quality are mandatory prerequisites for the safe implantation of this stem[14]. Similarly, the Nanos stem, an early representative of calcar-guided short stems, features narrowing in the distal section of the stem, primarily intended to allow proximal fixation, at the same time limiting the option of additional diaphyseal anchorage (Figure 8B).
Figure 7 Metaphyseal anchoring using three-point fixation.
A: Mayo stem (Zimmer Biomet, Warsaw, Indiana, USA); B: Metha stem (Aesculap, Tuttlingen, Germany); C: Nanos stem (Smith&Nephew, Marl, Germany).
Figure 8 Characteristics of various short stem designs at different CCD angles, according to the classification of Groups A–E established by Kutzner etal[22,35].
A: Metha stem (Aesculap, Tuttlingen, Germany); additional diaphyseal anchorage is almost impossible to attain; B: Nanos stem (Smith&Nephew, Marl, Germany); narrowing in the distal part limits the option of additional diaphyseal anchorage; C: Optimys stem (Mathys Ltd., Bettlach, Switzerland); in neutral and valgus positions, an additional diaphyseal anchorage is possible, when intended. (Copyright Mathys Ltd., Bettlach, Switzerland).
In new-generation, calcar-guided, short-stem THA, in addition to individualized positioning, the anchoring type can be individualized. When using the optimys stem in a varus position, a classical three-point anchoring approach should be attempted (Figure 2A). In the neutral and valgus position, an additional diaphyseal anchorage is possible (Figure 2B). In varus hips, the high level of the osteotomy proximal wedging combined with the three-point anchoring approach is typically sufficient, whereas in valgus hips, due to the low resection level, the stems may require an additional diaphyseal anchorage to achieve primary stability[34] (Figure 8C). Changing the type of anchorage through the addition of a diaphyseal anchorage will potentially result in negative effects on proximal bone remodeling and stress shielding compared with metaphyseal anchorage alone[21,34]. However, the option of additional individualized anchorage types increases the potential indications for the safe use of a short stem. The design features of calcar-guided short stems, including the ability to apply individualized meta-diaphyseal anchorages, may account for advantages of this stem type compared with earlier short-stem designs in terms of indications for use, including reduced quality of bone, osteonecrosis of the femoral head (ONFH), and femoral neck fractures[35-37].
BONE REMODELING
Due to distinct differences in the manifestation of bone remodeling, Yan et al[19] concluded in a recent review analysis that short stems should not be treated as one single implant group because periprosthetic bone loss is highly dependent on each particular stem design. The Metha stem has been associated with bone loss in the calcar region, whereas the Nanos stem presented bone resorption primarily in the greater trochanteric region, and these differences may be due to differences in the stem designs. Compared with conventional stems, such as the CLS stem (Zimmer Biomet, Warsaw, Indiana, USA) and the Bicontact stem (Aesculap, Tuttlingen, Germany), the study by Yan et al[19] also indicated that most short stems were associated with an overall lower rate of bone remodeling. A recent dual-energy X-ray absorptiometry study reported by Hochreiter et al[38] evaluated bone remodeling around the calcar-guided optimys stem. Bone mineral density increased primarily in the lateral region (Gruen zones 2 and 3) and the distal-medial region (Gruen zone 5), suggesting lateral loading. Thus, stress-shielding was limited, and periprosthetic bone loss was minimized when using this stem design.
Typical signs of diaphyseal stress, such as cortical hypertrophy, are commonly observed during the use of several conventional stem designs, frequently resulting in thigh pain. Cortical hypertrophy was commonly observed with the Fitmore stem (Zimmer Biomet, Warsaw, Indiana, USA)[39], whereas a low rate of distal bone remodeling associated with cortical hypertrophy has been reported for the calcar-guided optimys stem[33]. Almost all new-generation short stems present with a polished tip to reduce peak stresses and to prevent distal ingrowth (Figure 1).
MIGRATION AND SECONDARY STABILITY
The reduction in the length and diaphyseal fixation of the femoral component in short-stem THA may cause some concerns. A concomitant reduction of implant stability and an increase in interface micromotion might interfere with osteointegration, increasing the risk of aseptic loosening[17], which is likely to have crucial effects on long-term outcomes and revision rates. Whether this new group of stems will perform as well as conventional stems, which have a 25-year survival rate of 60%, cannot yet be predicted[40]. Studies investigating the migration patterns of modern short stems using EBRA-FCA (Ein-Bild-Roentgen-Analyse; femoral component analysis) have suggested an initial, pronounced settlement into the metaphyseal bone upon the initiation of full weight-bearing, followed by a subsequent stabilization[41-46]. In a recent investigation, most of the investigated stems showed delayed settlement during the first 2 years after surgery, suggesting that these new-generation stems are likely to display different migration patterns from conventional stems[34]. Male patients and heavy-weight patients have been shown to be at higher risk of subsidence, as are stems with valgus alignment[41]. Recent studies using radiostereometric analyses (RSA) have confirmed these findings. De Waard et al[47] reported the occurrence of secondary stabilization after initial migration using the optimys stem, suggesting a low risk of long-term aseptic loosening. Similarly, the mid-term results reported by the prospective RSA study performed by Floerkemeier et al[48] using the Metha stem showed no correlation between a greater initial migration and inferior clinical outcomes and no increased risk of aseptic loosening.
A securely achieved cortical contact with the distal lateral cortex appears to be crucial to provide sufficient primary stability[49] (Figure 8). A missing cortical contact has previously been defined as “undersizing”[49]. The use of intraoperative imaging to identify the potential “undersizing” of calcar-guided short stems is highly recommended, especially with regard to individualized positioning[20,50]. If the cortical contact is not securely achieved with the trial components, the stem should be upsized. At the mid-term, no clinically negative consequences were obvious in terms of implant survival[15,34]. Long-term results should, however, be obtained to further determine the impacts of early migration on secondary stability and short stem survival.
INDICATIONS
Short stems have been developed for use in young and active patients. To date, this group of patients continues to be primarily treated with short-stem THA. The most frequent indications for short-term THA are primary and secondary osteoarthritis; however, indications have constantly been expanded during recent years. To date, little clear evidence is available regarding the indications and contraindications of short stem use due to the limited availability of data.
Several short stems have been reported to be suitable for use in patients with developmental dysplasia of the hip joint[15,51-53]. While investigating the calcar-guided short stem MiniHip, Buttaro et al[54] found a survival rate of 100% at 5 years, using revision for aseptic loosening as the end point. They concluded that this stem design was well suitable for patients with hip dysplasia, producing only a few intraoperative technical problems.
Undoubtedly, the quality of the femoral bone stock plays a crucial role in the safe use of calcar-guided short stems. A recent multicenter investigation found a significantly increased periprosthetic fracture rate in patients with Dorr type C femora compared with those with Dorr type A and B femora[35]. Thus, the indication for use should be limited to Dorr type A and B. However, as the rates of stem revision did not differ significantly between younger and older patients; therefore, advanced age alone is not necessarily a contraindication for the use of calcar-guided short-stem THA, although longer follow-up has yet to be obtained[35].
The opportunity to intentionally choose an additional fit-and-fill in the proximal diaphysis associated with some calcar-guided short-stem designs potentially accounts for advantages compared with other short stems, particularly in terms of the broad range of indications associated with the use of these short stems. In addition to the classical short-stem philosophy of metaphyseal anchorage (Figure 9A), the same patient can also be treated by adding a fit-and-fill in the proximal diaphysis, if desired, such as in cases of reduced bone quality (Figure 9B). Generally, in these cases, the stem requires some degree of upsizing.
Figure 9 The same patient can be planned and treated by the application of metaphyseal anchorage or the addition of a fit-and-fill in the proximal diaphysis by valgization and upsizing, depending on the indication and bone quality.
A: Metaphyseal anchorage; B: Additional fit-and-fill in the proximal diaphysis.
The indication of ONFH in short-stem THA is controversial. The potentially reduced bone quality and the osteonecrotic area beyond the femoral head may also affect the femoral neck and the metaphyseal bone, and metaphyseal anchoring designs may be associated with poor primary stability and impaired osteointegration, which can jeopardize implant survival. For example, Schnurr et al[55] compared the use of the Metha stem in patients with ONFH with its use in patients with primary osteoarthritis over a 10-year period. They found that the aseptic loosening rate was significantly elevated among patients with ONFH. Recently, Afghanyar et al[36] reported a survival rate of 100% at the mid-term for the calcar-guided optimys stem in patients with ONFH. The findings strongly support the safe use of calcar-guided short stems for the treatment of patients with ONFH (Figure 10), providing sufficient primary stability and successful osteointegration. Further data on different calcar-guided short stems have confirmed these findings[56,57].
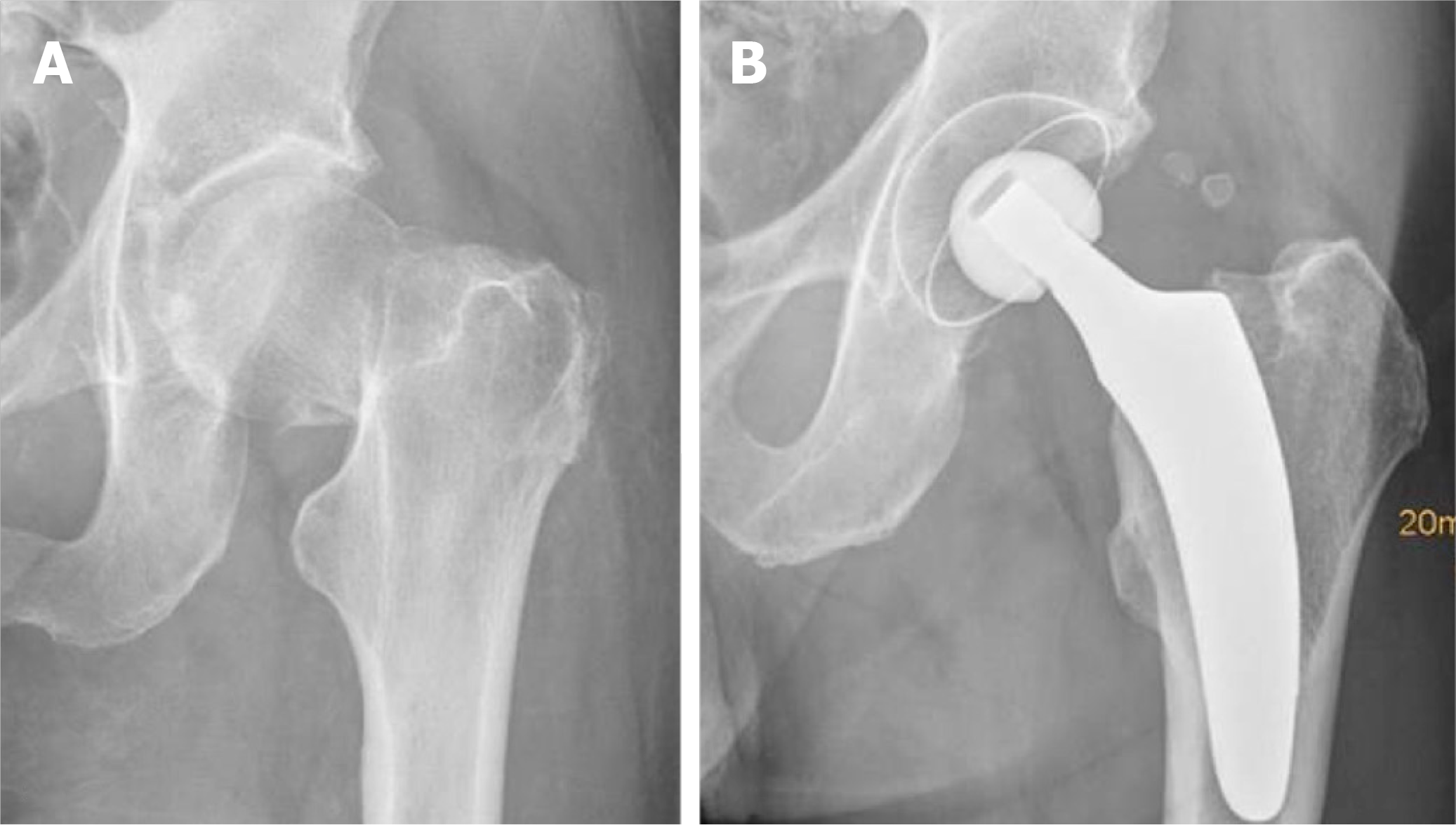
Figure 10 Calcar-guided short stem total hip arthroplasty in a case of osteonecrosis of the femoral head.
A: Preoperative; B: Postoperative.
To date, little evidence regarding the use of short cementless femoral components in cases of femoral neck fractures is available. However, Schneider et al[37] reported promising results using a calcar-guided short stem in patients with a femoral neck fracture who were active, characterized by Dorr type A or B femora, and provide an intact cortical ring of the femoral neck (Figure 11). A total of 16% of patients who required treatment due to femoral neck fracture were found to be eligible for this stem design, and a low complication rate was reported. However, the study has not come to an end yet. Two additional studies are available in the literature that investigated shorter stem designs in patients with femoral neck fractures, which reported encouraging outcomes; however, both stem designs were classified as shortened conventional stems (Group 4) based on the system established by Khanuja et al[58,59].
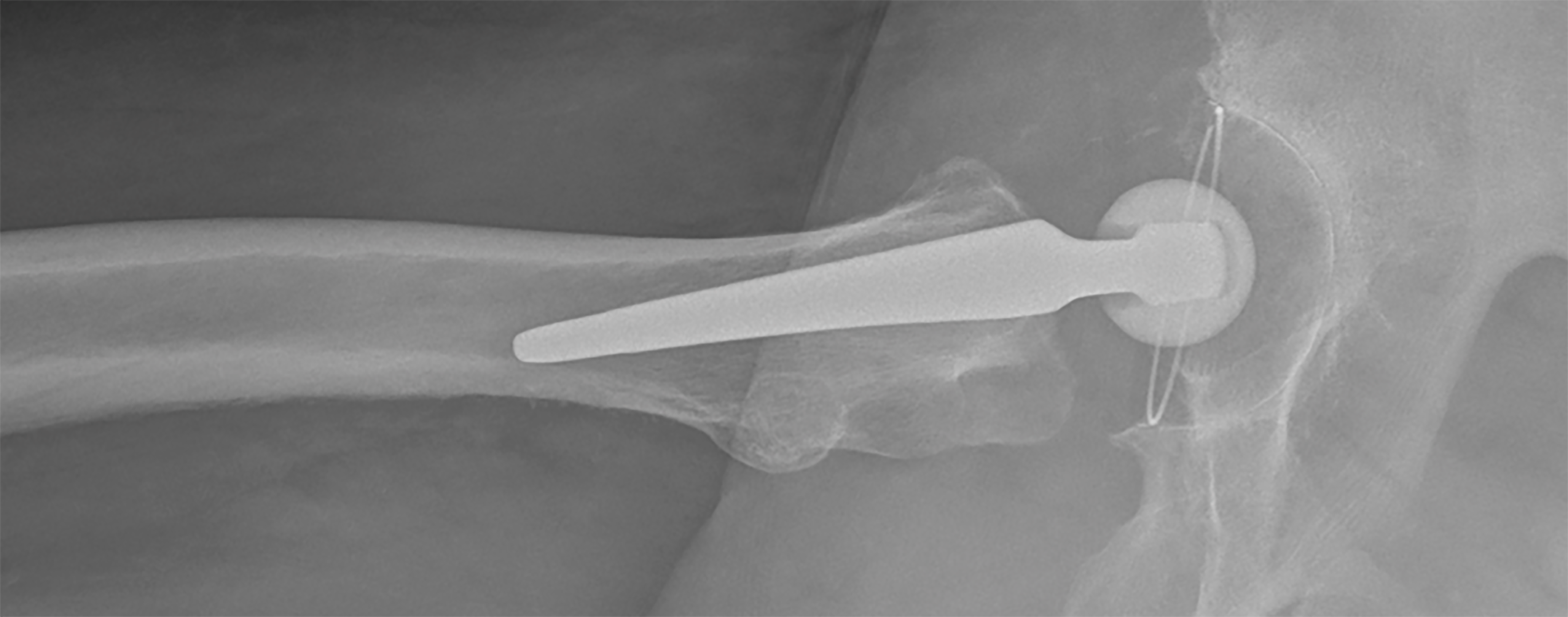
Figure 11 Calcar-guided short stem total hip arthroplasty in a case of a femoral neck fracture.
A: Preoperative; B: Postoperative.
Cemented short-stem THA may represent a potential alternative for patients with poor bone quality and osteoporosis, such as Dorr type C femora. To date, however, no new-generation short stem THA with cemented fixation are available on the market. Using prototypes of the optimys stem fabricated using polished steel (Figure 12), a recent in vitro biomechanical study demonstrated that the concept of a line-to-line cementation technique could be further pursued for the development of a cemented short stem in THA[60]. This finding was confirmed in a validated, computed tomography-based, finite element analysis performed by Azari et al[61] that quantified the mechanical performance of this short stem design. The results suggested that cemented short stems are a promising alternative for use in osteoporotic bone and may, therefore, further expand the range of indications in the future.
Figure 12 Prototype of a cemented calcar-guided short stem made out of polished steel (optimys stem, Mathys Ltd., Bettlach, Switzerland).
Copyright Mathys Ltd., Bettlach, Switzerland.
REGISTRY DATA
In recent years, short stems have increasingly been involved in national arthroplasty registries. The results of several national registries indicate that calcar-guided short stems are among the most successful implants in terms of early-stage survivorship. For example, in the German national joint registry, calcar-guided short stems, such as the optimys stem, the Nanos stem, the A2 stem, and the MiniHip stem, have been associated with excellent implant survival[10]. These results are strongly supported by findings from the Australian and the Swiss national registries, which provided similar results for these implant designs[62,63]. However, only mid-term registry data are currently available.
CONCLUSION
Modern calcar-guided short-stem THA offers numerous advantages compared with conventional THA. The broad potential to reconstruct the individual anatomical hip geometry, the reduction in proximal bone remodeling, and the simplified soft-tissue-sparing implantation represent true accomplishments. In Europe and globally, this group of implants is likely to become increasingly popular. Although this group of implants is still young, a large body of evidence has been obtained. The short- and mid-term outcomes are encouraging, although long-term results remain scarce.
If the long-term results confirm the promising early data, the option to anchor the femoral implant individually and the associated broad range of indications are likely to strongly favor calcar-guided stem designs as the future standard in THA. However, standard procedures, in general, should be easy to implement, reproducible, and practicable for every surgeon, regardless of technical expertise or surgical experience. The individualized implantation technique, however, requires distinct knowledge of the characteristics associated with varus and valgus positioning and the consequences of different types of anchoring, resulting in a significant learning curve for surgeons new to this technique, which must be considered. Contraindications to the use of these implants should be respected. Thus, improving education and collecting further clinical evidence will be crucial determinants of the future of calcar-guided short-stem THA.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Germany
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fujino T S-Editor: Wang JL L-Editor: A P-Editor: Xing YX